Access coupon
Patient self-testing
For the right patients, INR self-testing can result in improved time in the therapeutic range and superior therapy quality.

Patient self-testing is a better use of everyone’s time
Monitoring your warfarin patients’ PT/INR is essential for effective anticoagulation management. It enables necessary dose adjustments to be made to help increase their time in therapeutic range, but for many patients this can mean a lot of visits to the clinic or hospital.
Self-testing with the CoaguChek® INRange or CoaguChek® XS systems allows patients to measure their PT/INR themselves, anytime they like. Compared to usual care, where patients need to visit the clinic or hospital for a venous blood sample which is then sent to a laboratory for analysis, this gives patients more freedom and more time to themselves.1,2
Patients who self-test can share their PT/INR results on a regular basis, enabling you to closely monitor their PT/INR and make necessary dose adjustments without waiting for laboratory results.3,4

Patient self-testing gives you faster results for immediate treatment decisions, allowing for a more streamlined approach to monitoring, compared to usual care routines with venipuncture and laboratory INR testing.5–9
This could mean more workflow efficiency and less overcrowding at your clinic.6,10 Also, the more your patients self-test at home, the more time you can dedicate to other important work.
Self-testing can lead to improved patient engagement
In addition to saving time, self-testing can also motivate patients to become more involved in their own care.11,12
In a study of 2,922 warfarin patients, 87% of those randomized to self-testing adhered to their prescribed testing frequency compared with 52% of those who attended clinic appointments for testing.13
The CoaguChek® INRange system provides accurate PT/INR results in less than a minute and can be used by patients of all ages.3,11,13–16
With a short training session, your patients can learn to test themselves with ease and confidence. In fact, studies have shown that approximately three quarters of suitable patients can be taught how to correctly measure their own PT/INR values.14,15
Adherence to prescribed monitoring frequency13
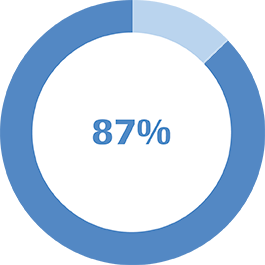
Self-testing patients
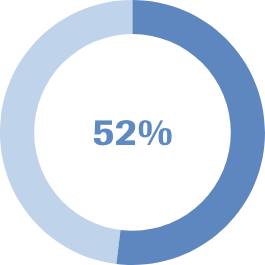
In-clinic
(usual care) patients
With patient self-testing, 87% of those randomized to self-testing adhered to their prescribed testing frequency compared with 52% of those who attended clinic appointments for testing.
Optimized VKA management
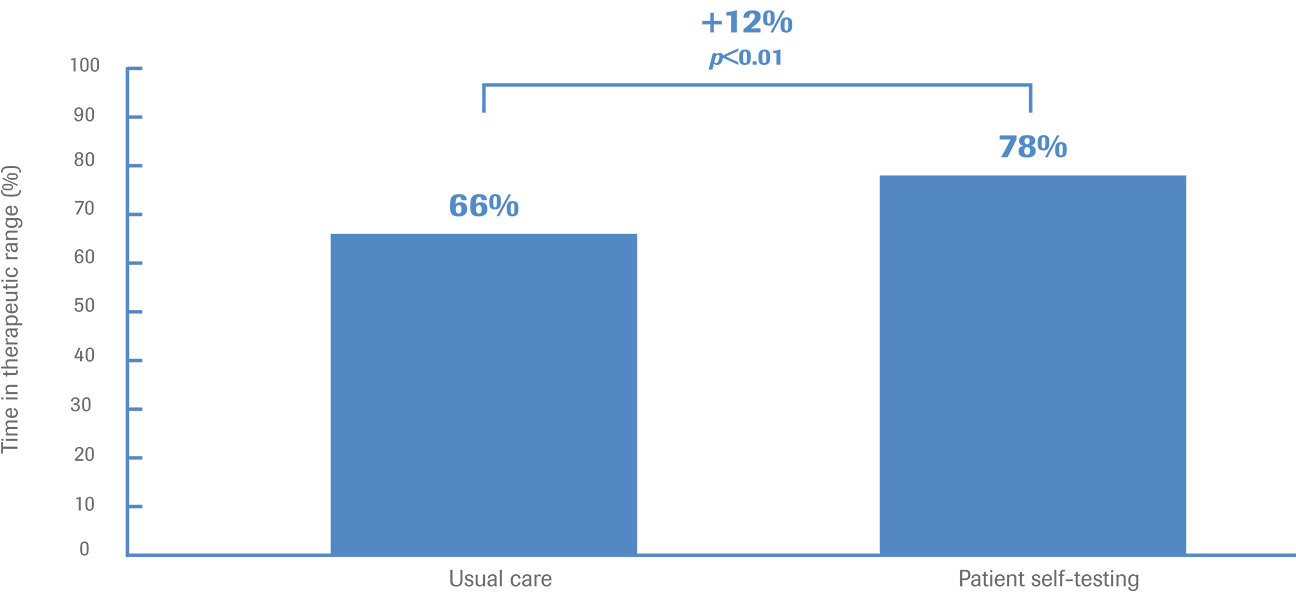
With PST, any necessary adjustments to your patients’ warfarin dosage can be made sooner than if they had to visit the clinic for testing. This can give them more time in therapeutic range and provide a more efficient means of warfarin monitoring and management.3,4,17
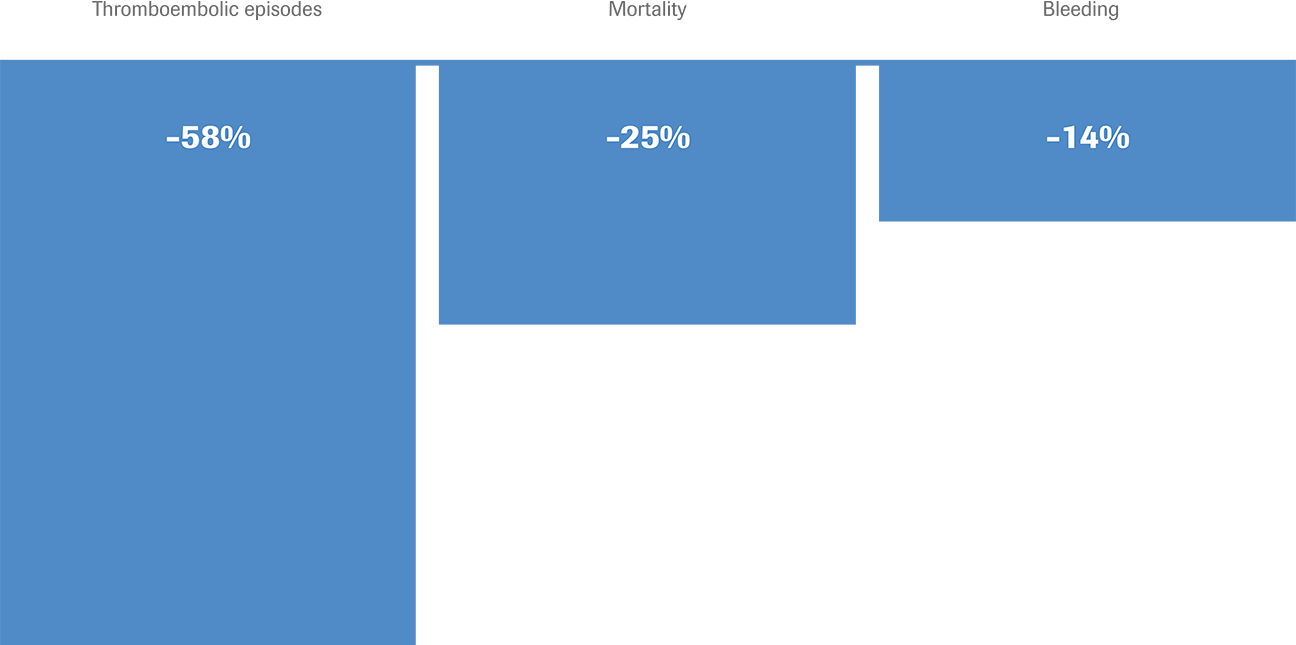
Patients who monitor their own PT/INR spend more time in therapeutic range compared with VKA patients who are tested in the laboratory or clinic. This can decrease the risk of adverse events for patients who self-test.3,4,17–19
More time (%) within the therapeutic range: Patient self-testing vs. usual care20
Reduction of complications and mortality with self-testing compared with routine monitoring
Prescribing considerations: Factors that influence the suitability of patient self-testing
Any patient who requires lifelong oral anticoagulants and is in a suitable cognitive and physical condition can learn how to self-test. A meta-analysis has shown that the patient’s age is not an obstacle and that self-testing is a safe option for all age groups.16
Patient self-testing may even be a particularly good option for older patients. During the training session, the qualified medical instructors deal with patient questions and individual requirements in a highly focused manner. Training sessions are also open to family members and caregivers.
Furthermore, patients can call the CoaguChek® Roche Care Centre for qualified advice and answers to any questions they have.
In order to make sure that patients have as little trouble as possible getting coverage from their health insurance, we recommend that your prescription include as many details and medical reasons for the prescription as possible.
More about reimbursement

Read our patient profiles
For additional factors to consider when deciding whether self-testing is right for your patient, read our patient profiles.
Meet Bruce and DorothyMaintaining oversight of patients who self-test
Even after becoming a coagulation self-tester, your patient will remain under your care. The concept of patient self-testing explicitly stipulates continuing care by the treating physician, and patients’ INR measurements are discussed during their quarterly appointments.
These discussions with independent patients can lead to closer relationships.
Training patients to self-test

Do you have questions about patient self-testing?
Visit our FAQ page for answers, or contact the CoaguChek® Roche Care Centre.
FAQs Contact usReferences:
- Nagler M et al. J Thromb Haemost. 2013;11:197–199.
- National Institute for Health and Care Excellence. NICE diagnostics guidance DG14. Available from: http://www.nice.org.uk/guidance/DG14. Accessed August 2016.
- Sharma P et al. Health Technol Assess. 2015;19:1–172.
- Bloomfield H.E et al. Ann Intern Med. 2011;154:472–482.
- Wurster M et al. Dis Manag. 2006;9:201–209.
- Larsson A et al. Ups J Med Sci. 2015;120:1–10.
- Ryan F et al. Thromb Res. 2010;126:e345-e348.
- Gubala V et al. Anal Chem. 2012;84:487–515.
- Bereznicki L.R.E et al. J Med Internet Res. 2013;15:e138.
- Huston T. Med Lab Obs. 2009;41:28–30.
- Gardiner C et al. Br J Haematol. 2005;128:242–247.
- Burgwinkle P et al. Managed Care. 2008;17(Suppl 9):1–8.
- Matchar D.B et al. N Engl J Med. 2010;363:1608–1620.
- Connock M et al. Health Technol. 2007;Assess 11(38):iii–iv, ix-66.
- Dolor R.J et al. J Thromb Thrombolysis. 2010;30:263–275.
- Heneghan C et al. Lancet 2012;379(9813):322–334.
- Heneghan C.J et al. Cochrane Database Syst Rev. 2016;7;CD003839.
- Khan T.I et al. Br J Haematol. 2004;126:557–564.
- Heneghan C et al. Lancet 2006;367:404–411.
- Holbrook A et al. Chest 2012;141;e152S–e184S.